Mobile Multispectral Near-Infrared Spectroscopy Imaging for Evidence-Based Skin Graft Flap Assessment
- By Wish Clinic
- In Articles
Introduction
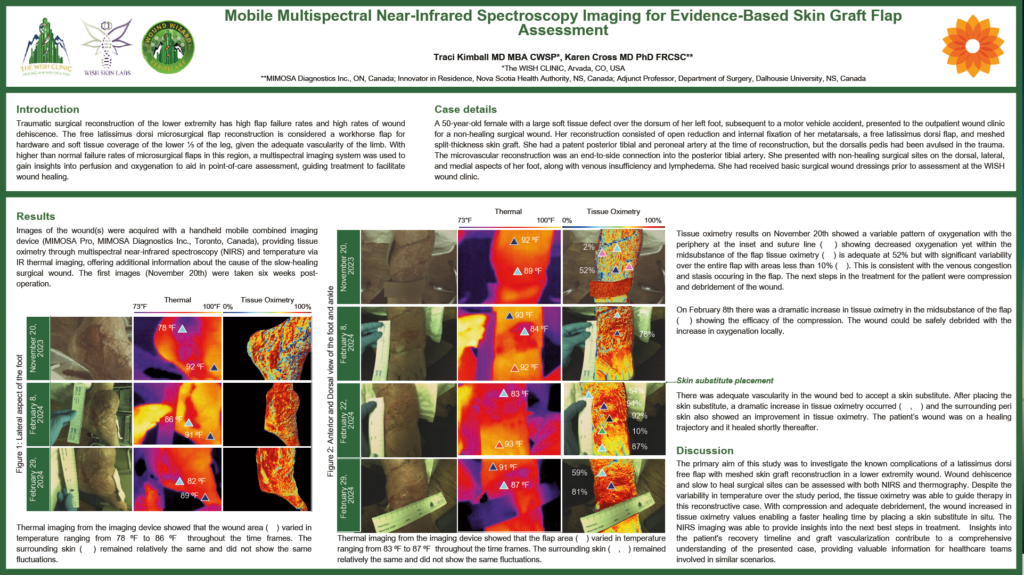
Traumatic surgical reconstruction of the lower extremity has high flap failure rates and high rates of wound dehiscence. The free latissimus dorsi microsurgical flap reconstruction is considered a workhorse flap for hardware and soft tissue coverage of the lower ⅓ of the leg, given the adequate vascularity of the limb. With higher than normal failure rates of microsurgical flaps in this region, a multispectral imaging system was used to gain insights into perfusion and oxygenation to aid in point-of-care assessment, guiding treatment to facilitate wound healing.
Traci Kimball MD MBA CWSP*, Karen Cross MD PhD FRCSC** *The WISH CLINIC, Arvada, CO, USA **MIMOSA Diagnostics Inc., ON, Canada; Innovator in Residence, Nova Scotia Health Authority, NS, Canada; Adjunct Professor, Department of Surgery, Dalhousie University, NS, Canada
Case details
A 50-year-old female with a large soft tissue defect over the dorsum of her left foot, subsequent to a motor vehicle accident, presented to the outpatient wound clinic for a non-healing surgical wound. Her reconstruction consisted of open reduction and internal fixation of her metatarsals, a free latissimus dorsi flap, and meshed split-thickness skin graft. She had a patent posterior tibial and peroneal artery at the time of reconstruction, but the dorsalis pedis had been avulsed in the trauma.
The microvascular reconstruction was an end-to-side connection into the posterior tibial artery. She presented with non-healing surgical sites on the dorsal, lateral, and medial aspects of her foot, along with venous insufficiency and lymphedema. She had received basic surgical wound dressings prior to assessment at the WISH wound clinic.
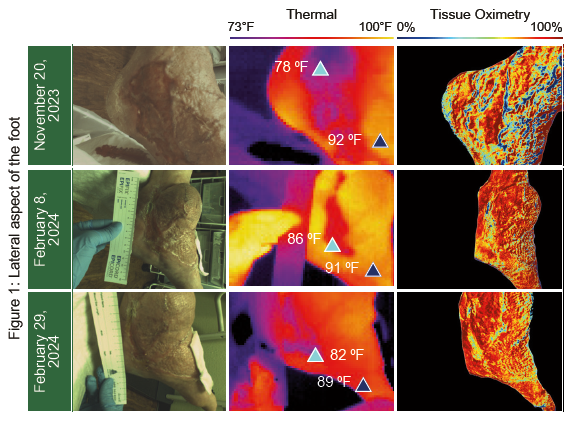
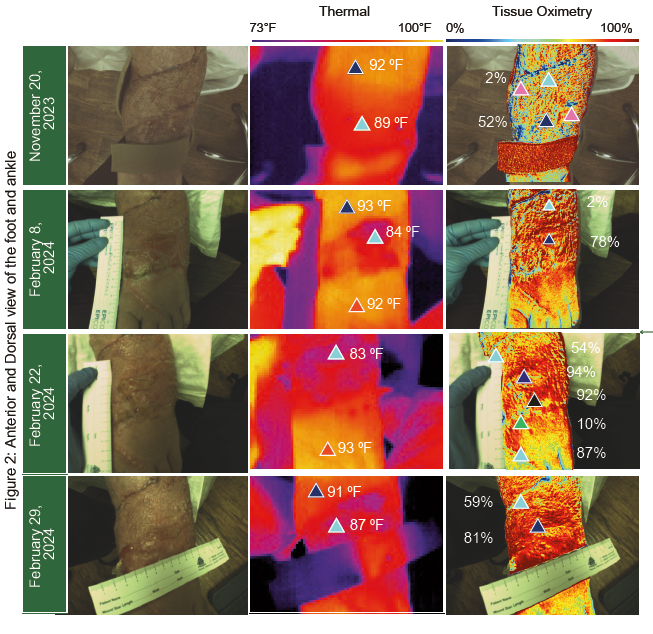
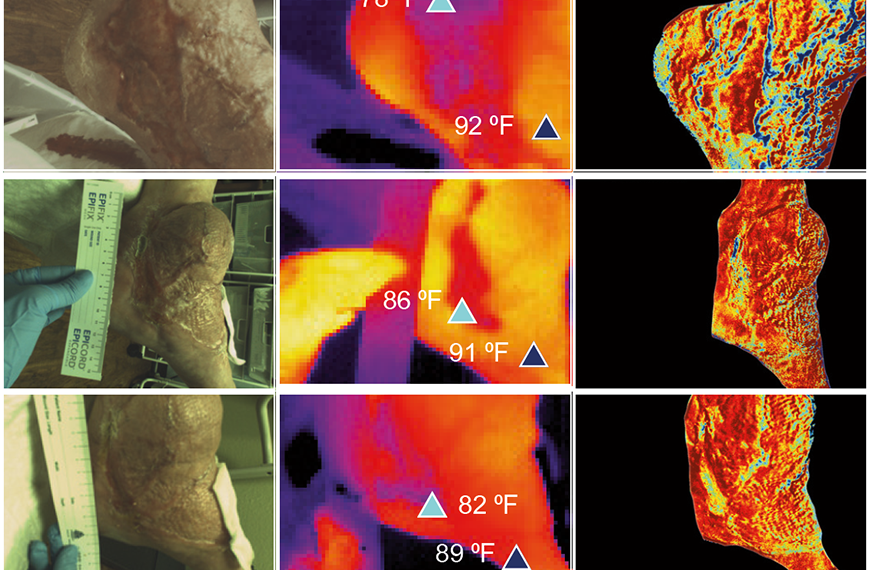
Tissue oximetry results on November 20th showed a variable pattern of oxygenation with the periphery at the inset and suture line ( ) showing decreased oxygenation yet within the midsubstance of the flap tissue oximetry ( ) is adequate at 52% but with significant variability over the entire flap with areas less than 10% ( ). This is consistent with the venous congestion and stasis occurring in the flap. The next steps in the treatment for the patient were compression and debridement of the wound.
On February 8th there was a dramatic increase in tissue oximetry in the midsubstance of the flap ( ) showing the efficacy of the compression. The wound could be safely debrided with the increase in oxygenation locally.
Skin substitute placement
There was adequate vascularity in the wound bed to accept a skin substitute. After placing the
skin substitute, a dramatic increase in tissue oximetry occurred ( , ) and the surrounding peri
skin also showed an improvement in tissue oximetry. The patient’s wound was on a healing
trajectory and it healed shortly thereafter.
Discussion
The primary aim of this study was to investigate the known complications of a latissimus dorsi free flap with meshed skin graft reconstruction in a lower extremity wound. Wound dehiscence and slow-to-heal surgical sites can be assessed with both NIRS and thermography. Despite the variability in temperature over the study period, the tissue oximetry was able to guide therapy in this reconstructive case. With compression and adequate debridement, the wound increased in tissue oximetry values enabling a faster healing time by placing a skin substitute in situ. The NIRS imaging was able to provide insights into the next best steps in treatment. Insights into the patient’s recovery timeline and graft vascularization contribute to a comprehensive understanding of the presented case, providing valuable information for healthcare teams involved in similar scenarios.
You may also like
Vascular Assessment for Diabetic Wounds | WISH Clinic
- January 27, 2026
- by Wish Clinic
- in Articles

Role of Glucose Control in Wound Healing | The WISH Clinic

Neuropathy Pain Relief, Symptoms, Causes, and Treatment Options