Medicare Changes and Their Impact on Wound Care Patients and Providers
- By Wish Clinic
- In Articles
Medicare Changes and Their Impact on Wound Care Patients and Providers
The healthcare landscape is constantly evolving, and Medicare changes are some of the most significant shifts affecting patients and providers alike. For those managing chronic wounds—or healthcare professionals providing wound care services—understanding these changes is essential. Let’s explore how upcoming Medicare policies will impact wound care treatments, coverage, and reimbursement processes.
What Are the Upcoming Medicare Changes?
When we talk about Medicare changes, we’re referring to policy adjustments across Medicare Parts A, B, C, and D that can affect everything from hospital stays to prescription coverage. Proposed reforms, particularly under initiatives like Project 2025, are designed to streamline costs and improve patient care. However, for those needing specialized wound care, these changes could significantly alter access to critical treatments.
Key Medicare Parts and Their Role in Wound Care
Medicare Part A: Hospital Insurance
Covers inpatient hospital stays, skilled nursing facilities, and home health care. For wound care patients, this includes surgeries for wound debridement, hospital stays related to infection management, and wound care provided in skilled nursing facilities.
Medicare Part B: Medical Insurance
Covers outpatient care, including doctor visits, preventive services, and durable medical equipment (DME). This is crucial for wound care patients needing advanced dressings, compression garments, and negative pressure wound therapy (NPWT) devices.
Medicare Part C: Medicare Advantage
A private insurance alternative to traditional Medicare. Medicare Advantage plans can offer additional benefits but often come with network restrictions that may impact a patient’s ability to see wound care specialists.
Medicare Part D: Prescription Drug Coverage
Covers medications needed to manage wound-related infections, pain, and underlying conditions like diabetes that contribute to chronic wounds.
How Medicare Changes Will Affect Wound Care Coverage
Changes to Reimbursement Policies
One of the biggest shifts involves adjustments to reimbursement rates for wound care procedures and supplies. Medicare currently covers advanced wound care treatments like hyperbaric oxygen therapy (HBOT) and NPWT, but proposed changes may reduce reimbursement rates for these costly treatments.
Telemedicine and Wound Care
During the COVID-19 pandemic, telehealth services became essential for patients with mobility issues or those in rural areas. However, Medicare’s future telemedicine policies remain unclear. If coverage for telemedicine visits is reduced, patients with chronic wounds who rely on remote consultations may face challenges accessing care.
Coverage for Wound Care Supplies
Medicare Part B currently covers durable medical equipment (DME) and wound care supplies, but proposed Medicare changes could limit what’s included. This would impact patients needing advanced dressings, compression garments, and wound irrigation systems.
Real-World Example: The Cost of Advanced Wound Care
Consider Sarah, a diabetic patient managing a chronic foot ulcer. Her wound requires negative pressure wound therapy (NPWT) and regular visits to a wound care specialist. Under current Medicare rules, Sarah’s NPWT device and doctor visits are covered. However, proposed Medicare changes could increase her out-of-pocket costs, making it harder for her to afford the necessary care.
What Healthcare Providers Need to Know
For healthcare providers, Medicare changes mean adapting to new reimbursement rates and coverage rules. Understanding these changes is essential to ensure compliance and maintain patient care quality.
- Stay updated on Medicare policies
- Review reimbursement adjustments
- Advocate for patients facing coverage limitations
FAQs About Medicare Changes and Wound Care
Will Medicare still cover advanced wound care treatments?
It depends on the specific changes implemented. While traditional Medicare currently covers many treatments, Medicare Advantage plans may have different policies.
How can patients ensure their wound care is covered?
Patients should review their Medicare plans annually and consult with their providers to understand coverage details.
Are there financial assistance programs for wound care?
Yes, some organizations offer financial aid to help patients cover the costs of wound care treatments.
Practical Takeaways for Wound Care Patients
To navigate Medicare changes effectively, wound care patients should:
- Stay informed about upcoming policy changes
- Review their Medicare plans annually
- Consult their healthcare providers about coverage options
If you have questions about how Medicare changes may impact your wound care, contact The WISH Clinic in Arvada, CO, for expert advice and care.
Call us at: 303-940-1611
Email us at: info@thewishclinic.com
Your health matters, and access to the right care is essential for recovery and quality of life.
You may also like
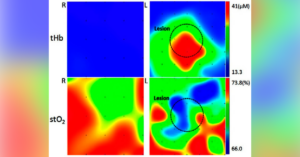
Near Infrared Spectroscopy: A Game-Changer in Wound Care
- March 20, 2025
- by Wish Clinic
- in Articles

Revolutionizing Wound Care: Innovative Treatments at The WISH Clinic